We all know at least one woman – maybe even yourself – who gets anxious at the thought of jumping jacks, squat jumps, sprints… and let’s not talk about trampolines!
As a women’s PT and group exercise instructor to mums, I’ve worked with and advised countless women with weakened pelvic floor muscles, many of whom have just carried on without seeking help as it’s something they just ‘learn to cope with’.
But given the prolific nature of women suffering from weakness to varying degrees (in the UK, 50% of mothers who had a vaginal birth will suffer from prolapse and 45% from urinary incontinence within seven years after giving birth), it’s sad to see the lack of awareness and education in this country.
But here’s the good news, most pelvic floor dysfunction is treatable through physical therapy, medication and biofeedback (where sensors are placed on the abdomen and anal canal to measure the electrical activity of the muscles that control bowel and bladder functions and inform you how to perform various movements correctly).
So if you start to experience any symptoms that are mentioned in this feature, speak to a specialist or GP as soon as possible. Early treatment can help to improve your quality of life and ease any discomfort or inconvenience. So let’s talk about what our pelvic floor actually is and what it does.
What is the pelvic floor?
The pelvic floor is made up of a group of muscles located in your pelvis. They stretch like a hammock from the pubic bone (at the front) to the coccyx or tailbone (at the back) and from side to side.
These muscles have a big job to do; they work alongside your internal abdominal and back muscles to offer stability to the spine and they also help to control pressure inside to manage the force when you lift or strain – such as heavy lifting or exercise. They maintain bladder and bowel control and play an important role in sexual sensation and function.
When the pelvic floor muscles are contracted, the internal organs lift and the muscular bands called sphincters tighten the opening of the vagina, anus and urethra. Relaxing these muscles allows for easy passage of urine and faeces.
What causes the pelvic floor to weaken?
Common causes of a weak pelvic floor are pregnancy, childbirth, obesity, straining of chronic constipations, constant coughing, lower levels of estrogen after menopause, tension caused by painful periods or endometriosis, or even family history and genetics can play a part.
Some symptoms include:
•
Leaking urine when coughing, sneezing, laughing or running.
• Failing to reach the toilet in time.
•
Passing wind from either the
anus or vagina when bending
over or lifting.
• Reduced sensation in the vagina.
• Tampons that dislodge or fall out.
•
A distinct bulge at the vaginal opening.
•
A sensation of heaviness in
the vagina.
•
A heaviness or dragging in the pelvis or back.
•
Recurrent urinary tract infections, or recurrent thrush.
•
Vulval pain, pain with sex, inability to orgasm.
What’s a prolapse?
A pelvic organ prolapse happens when the muscles and tissues supporting the organs (uterus, bladder and rectum) become weak or loose which allows one of those organs to drop, press into or out of the vagina. There’s a certain amount of suffering in silence with this condition due to embarrassment or thinking that the symptoms are ‘normal’. However, it is treatable.
There are different types of prolapse, depending on which pelvic organ has been affected.
The most common types include:
•
Dropped bladder (called cystocele). This happens when the bladder drops into or out of the vagina.
•
Rectocele. This happens when
the rectum bulges into or out
of the vagina.
•
Dropped uterus (uterine prolapse). This happens when the uterus bulges into or out of the vagina. Uterine prolapse is sometimes associated with small bowel prolapse (called enterocele),
where part of the small intestine, or small bowel, bulges into
the vagina.
If you experience any of the below symptoms you may be suffering from a prolapse:
•
Seeing or feeling a bulge or ‘something coming out’ of
the vagina.
•
A feeling of pressure, discomfort, aching or fullness in the pelvis.
•
Pelvic pressure that gets worse with standing or coughing or
as the day goes on.
•
Leaking urine (incontinence)
or problems having a bowel movement.
• Problems inserting tampons.
•
Discomfort during physical activity or sex.
If the symptoms are severe, treatments can include hormones, vaginal pessaries or even surgery. However, the first place to start is by making lifestyle changes and incorporating regular pelvic floor exercises.
The following exercises are designed to improve your muscle tone but also improve your brain connection as you focus on the internal holds and movements. Doing these exercises regularly may prevent any need for corrective surgery.
Which exercises can help treat or prevent a pelvic floor disorder?
Kegel exercises (aka pelvic squeezes)
1) Identify the muscles: Begin by finding the right muscles to engage. Imagine trying to stop the flow of urine or prevent passing wind. The muscles you engage in these actions are your pelvic floor muscles.
2) Correct technique: Once you have identified the muscles, contract them by squeezing and lifting. Hold the contraction for a few seconds, then release and relax. Aim for three sets of 10 repetitions, gradually increasing the duration of the holds as you gain strength. Try to include both short sharp squeezes as well as long holds.
3) Stay consistent: Make these exercises a part of your daily routine. Consistency is key.
Pelvic tilts
1) Lie on your back with your knees bent and feet flat on the floor.
2) Inhale deeply, then exhale
while gently flattening your lower back against the floor. Engage
your abdominal muscles during
this movement.
3) Hold for a few seconds, then release and relax.
4) Repeat for 10 to 15 reps, gradually increasing the duration of the holds as you progress.
Bridge pose
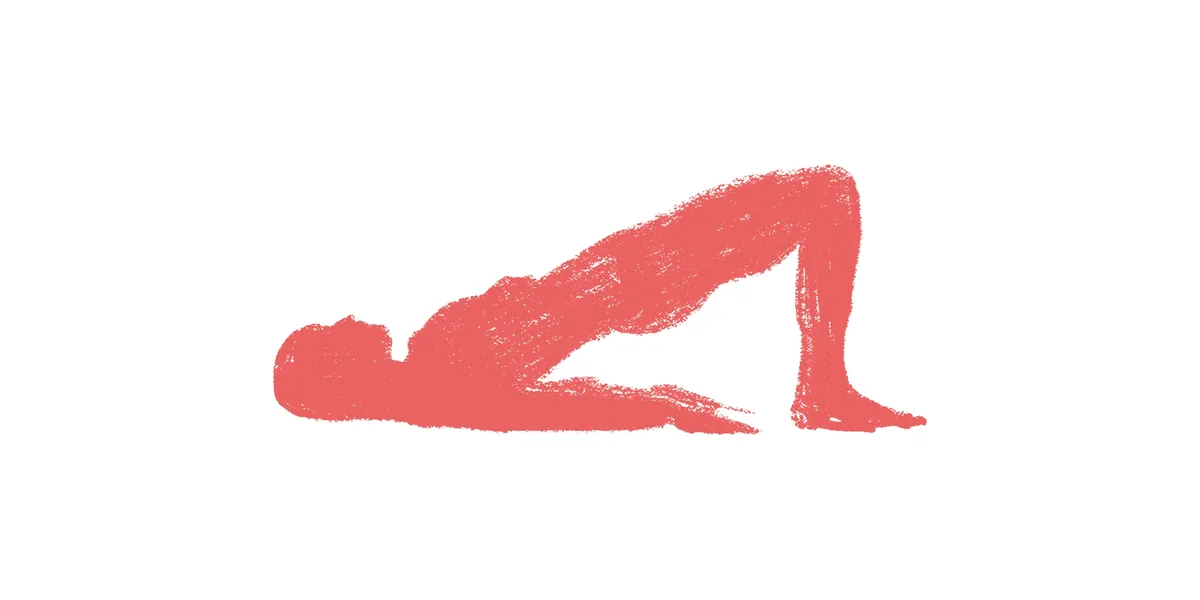
1) Lie on your back with your knees bent, feet flat on the floor, and arms by your sides.
2) Inhale deeply, then exhale as
you lift your hips off the floor, engaging your glutes and pelvic floor muscles.
3) Hold the bridge position for a few seconds, ensuring that your body forms a straight line from your shoulders to your knees.
4) Slowly lower your hips back
down to the starting position.
5) Repeat for 10 to 15 reps.
Squats

1) Stand with your feet
shoulder-width apart and
toes slightly turned out.
2) Inhale deeply, then exhale as you bend your knees and lower your hips, as if sitting back into a chair.
3) Coming back to stand, try to engage the pelvic floor muscles as
if squeezing and lifting a marble internally on the return to upright position, perhaps finishing with a slight pelvic tilt and release.
Takeaway Tips
- Do kegels/pelvic squeezes on a daily basis.
- Maintain a healthy balanced diet.
- Manage weight gain.
- Do not smoke as this affects tissues and may bring on a chronic cough increasing the risk of further strain.
- Avoid heavy lifting and activities that put excessive strain on the pelvic floor.
- Gradually increase the intensity of your regular exercises as you gain strength and confidence.
- Aim to incorporate at least a 30% activation of the pelvic floor where possible into your exercise (i.e. squats, lunges, low impact cardio, leg raises, medium to light weight work).
- Continue to incorporate pelvic floor exercises into your routine even after recovery to help prevent future issues and to maintain overall pelvic health – your pelvic floor will thank you!
Top image credit: Getty Images
