Let’s talk menopause and bone health. Thankfully, this natural transition we all go through in our later life is now less of a ‘closely-guarded secret’ and more of a ‘must-do talking point’, with many businesses and companies now offering support for women experiencing this often difficult stage in their lives.
Difficult because the symptoms are as varied as they are many – fatigue, hot flashes, dry skin, night sweats, irritability, weight gain, to name just a few in an ever-expanding catalogue. And which ones you get and for how long are anyone’s guess!
Bone density may not be the most talked-about menopausal ‘side effect’, but it’s certainly an important one to cover, particularly for athletes and those in training. So as we grow older, our exercise and nutrition must be adapted to the changes our bodies go through and to accommodate any potential reduction in bone density.
Menopause and bones: How are the two linked?
Menopause is the end of the reproductive phase in a woman’s life and is mainly characterised by a drop in the levels of oestrogen hormone. As our ovaries no longer produce it, it causes our menstrual cycles to stop and the above mentioned symptoms, and more, associated with menopause.
It’s the drop in this particular hormone which affects the activity of bone cells called osteoblasts, as they play a vital role in building new bone tissue. This is why women can lose up to 10% of their bone mass in the first five years after menopause, and can make women more susceptible to fractures and osteoporosis, affecting approximately 1 in 10 women over the age of 60 worldwide.
To explain a bit more, women reach their peak bone mass around the ages of 25 to 30, when the skeleton has stopped growing and our bones are at their strongest and thickest. Bone density is the measure of the amount of mineral content in bones, determining their strength and resilience.
A healthy bone has a honeycombed appearance whereas a bone that’s developed osteoporosis contains larger holes with a softer middle. This bone is weaker and vulnerable to breaking. In more severe cases, breaks might even occur after a mild knock, fall or bump.
Other factors contributing to a reduction in bone density include a lack of calcium, vitamin D (whch helps regulate the amount of calcium in the body), and physical activity. Smoking, excessive alcohol consumption, and certain medications, such as corticosteroids, could also exacerbate the loss.
But it’s the five years after menopause where we see the biggest acceleration.
What medications can or should we take?
The most common treatment subscribed to patients experiencing peri and postmenopausal symptons is HRT. It’s been proven to be effective at reducing the risk of a broken bone by increasing the level of hormones which an average woman would have.
There have been some health-risk concerns such as breast cancer, blood clots and stroke through taking HRT on a long-term basis, especially in older women who might have been at high risk to begin with.
However, evidence from recent trials have proven HRT to be generally safe and effective. After the age of 60, other bone strengthening medications can also be prescribed.
Which foods should be included in our diet?

A healthy diet is crucial to lessen the effects of menopause on bone density. A wide range of foods will give your bones all the nutrients they need, so make sure your diet includes fruit and vegetables; dairy (if no allergies); carbohydrates (pasta, bread, potatoes) and protein (meat, fish, eggs and pulses or beans).
The recommended nutritional intake of calcium per day for postmenopausal women is 1,200mg, and 10 micrograms (400 international units) of vitamin D a day. Sources of calcium include milk, cheese, yoghurt, sardines, pilchards, soya drinks, green leafy vegetables, pulses, tofu, and dairy-free milk.
Some women may need to take supplements to ensure they’re getting enough.
As the best source of vitamin D is direct sunlight, UK residents should take supplements (D3 is the more effective type) between October and early March.
It’s also advised to reduce alcohol intake to stay within the recommended limits and for smokers to seek help to stop.
Triathlete focus
Hydration is key as it becomes harder to handle the heat during this time of hormonal change. And save the simple sugars and starchy carbs for when you really need them during races and training, as your diminished oestrogen means you’re less insulin resistant and more sensitive to carbs, so you’re better off opting for fruit and veg.
Aim to get about 30g of carbs (about the amount in one banana) during a long endurance training session. This is generally proven to be sufficient according to exercise physiologist and nutritionist Stacy Sims, author of How to match your food and fitness to your unique female physiology for optimum performance and creator of ‘The Menopause for Athletes’ course.
She also recommends around 25g of protein within 30mins of a hard exercise session as high cortisol levels mean you’re more catabolic (when you’re eating into muscles for energy). Protein will bring down the cortisol and promote repair.
Sims adds: “Choose recovery foods such as Greek yoghurt, cottage cheese or a drink with whey and casein for the best result.”
What type of exercise helps?
To build strength in the bones, you need to do a combination of exercises where you bear weight on your feet and work your muscles harder than you normally would in your everyday activity. Bone is living tissue so when you bear weight on it, it gets stronger.
Studies have shown that regular weight-bearing exercises (i.e. 30-45mins three times a week) can help to improve bone density and reduce the risk of fractures in postmenopausal women.
Weight-bearing exercises are any type of activity which makes the body work against gravity while standing or moving. These help to stimulate bone growth by triggering osteoblasts to build new bone tissue. For example:
High impact
- Jogging/running
- Skipping rope
- Step aerobics
- Tennis
- Heavy lifting or pushing – e.g. shopping, gardening or heavy weight training in the gym (i.e. 3-6 reps to overload)
Moderate impact
- Dancing
- Hiking
- Stair/hill climbing
- Medium-heavy weights (i.e. 12-15 reps to overload)
Low impact
- Elliptical and stair step machines
- Low-impact aerobics
- Brisk walking
- Light weights (i.e. 20 reps or more to overload)
Functional strength and balance workouts can include basic moves such as calf raises, bodyweight exercises like press-ups or squats and using equipment such as resistance bands, free weights, and weight machines.
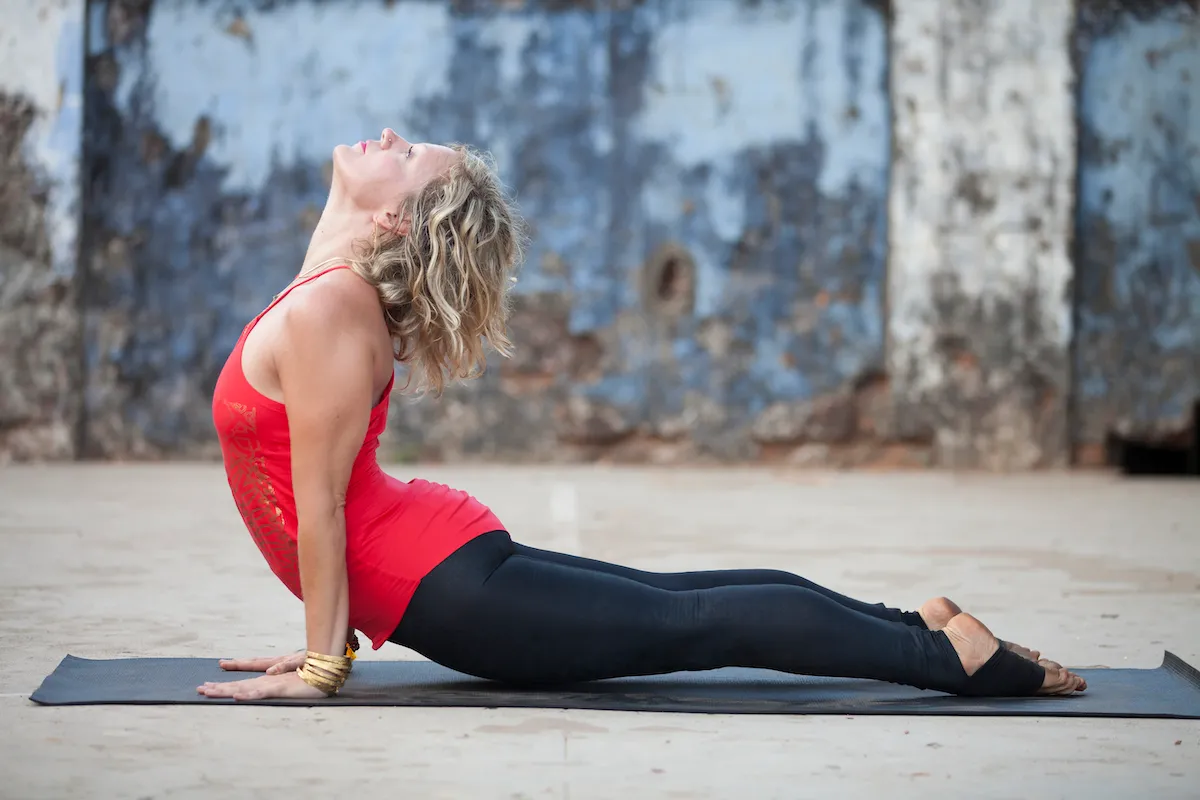
Yoga and Pilates can also improve strength, balance and flexibility in menopausal women, but some of the moves, such as bends, can make women with osteoporosis more susceptible to fractures, so always speak to a qualified instructor before starting.
Takeaway tips
1. Incorporate aerobic or cardiovascular activity (swimming, running and cycling) 2-3 times a week.
2. Add strength-training exercises to your workouts 2-3 days a week.
3. Include flexibility, stability and stretching exercises into your routine where possible.
4. Don’t forget to include mobility moves to warm up before a workout and a good stretch after a workout.
Top image credit: Getty Images
